Who have to measuring bone density through bone densitometer
Bone Densitometry
Osteoporosis is a significant loss of bone mineral density that affects millions of women, placing them at risk for potentially debilitating fractures. We offer bone densitometry, which precisely measures bone mineral density (BMD), allowing for estimation of a patient’s fracture risk. Our advanced system is capable of accurately calculating BMD in the spine, hip, or wrist. The system also permits determination of BMD in the pediatric population.
Your physician may order a bone densitometry if he or she suspects you have or are in danger of developing osteoporosis. People with osteoporosis have weak bones or a significant loss of their bone mineral density. Millions of women and many men develop osteoporosis as they age.
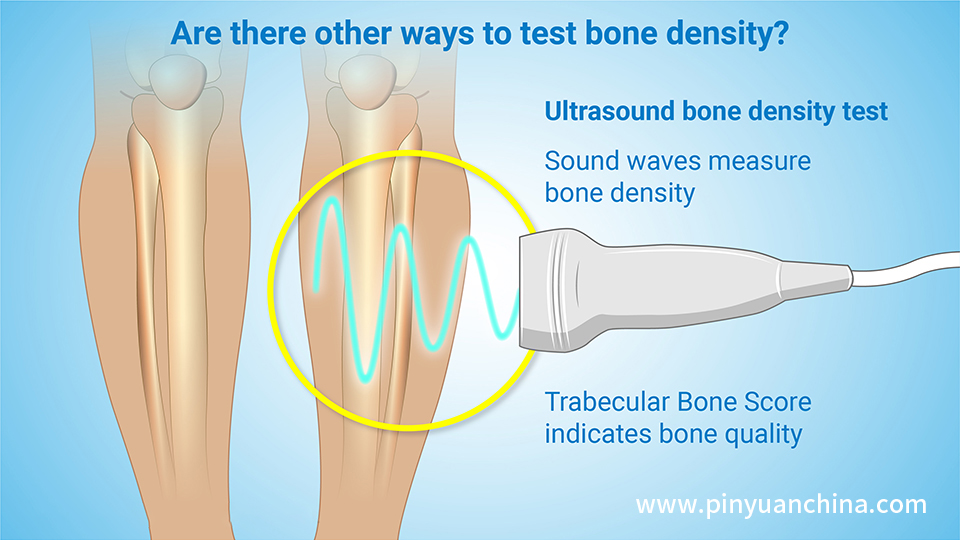
How Bone Densitometry Works
Sometimes this exam is called bone density scanning or dual-energy x-ray absorptiometry (DXA). It’s an enhanced form of x-ray technology. The DXA machine sends a thin, invisible beam of low-dose x-rays through the bones. Your soft tissues absorb the first energy beam. Your bones absorb a second beam. By subtracting the soft tissue amount from the total, the machine provides a measurement of your bone mineral density (BMD). That density tells the physician the strength of your bones.
Why Physicians Use Bone Densitometry
Osteoporosis involves a loss of calcium in your bones. It’s a condition that most often affects women after menopause, although men can have osteoporosis, too. Along with the calcium loss, the bones go through structural changes that cause them to become thinner, more fragile and more likely to break.
DXA also helps radiologists and other physicians track the effectiveness of treatments for any type of bone loss condition. The exam’s measurements give evidence about your risk of breaking a bone.
Who Should Receive Bone Mineral Density (BMD) Testing
• Women aged 65 and older
• Postmenopausal women under age 65 with risk factors for fracture.
• Women during the menopausal transition with clinical risk factors for fracture, such as low body weight, prior fracture, or high-risk medication use.
• Men aged 70 and older.
• Men under age 70 with clinical risk factors for fracture.
• Adults with a fragility fracture.
• Adults with a disease or condition associated with low bone mass or bone loss.
• Adults taking medications associated with low bone mass or bone loss.
• Anyone being considered for pharmacologic (drug) therapy.
• Anyone being treated, to monitor treatment effect.
• Anyone not receiving therapy in whom evidence of bone loss would lead to treatment.
• Women discontinuing estrogen should be considered for bone density testing according to the indications listed above.
Why Physicians Use Vertebral Fracture Assessment (VFA)
Another exam performed on the DXA machine is vertebral fracture assessment (VFA). It’s a low-dose x-ray examination of the spine that assesses your backbone health. A VFA will reveal whether you have compression fractures in your vertebra (the bones in your spine). The presence of a vertebral fracture is of even more value in predicting your risk of bones breaking in the future than DXA alone. The following are reasons (indications) for performing vertebral fracture assessment (VFA) based on the 2007 Official Positions of the International Society of Clinical Densitometry (www.iscd.org):
Who Should Receive VFA
• Postmenopausal women with low bone mass (osteopenia) by BMD criteria, PLUS any one of the following:
• Age greater than or equal to 70 years
• Historical height loss greater than 4 cm (1.6 in.)
• Prospective height loss greater than 2 cm (0.8 in.)
• Self-reported vertebral fracture (not previously documented)
• Two or more of the following;
• Age 60 to 69 years
• Self-reported prior non-vertebral fracture
• Historical height loss of 2 to 4 cm
• Chronic systemic diseases associated with increased risk of vertebral fractures (for example, moderate to severe COPD or COAD, seropositive rheumatoid arthritis, Crohn’s disease)
• Men with low bone mass (osteopenia) by BMD criteria, PLUS any one of the following:
• Age 80 years or older
• Historical height loss greater than 6 cm (2.4 in)
• Prospective height loss greater than 3 cm (1.2 in)
• Self-reported vertebral fracture (not previously documented)
• Two or more of the following;
• Age 70 to 79 years
• Self-reported prior non-vertebral fracture
• Historical height loss of 3 to 6 cm
• On pharmacologic androgen deprivation therapy or following orchiectomy
• Chronic systemic diseases associated with increased risk of vertebral fractures (for example, moderate to severe COPD or COAD, seropositive rheumatoid arthritis, Crohn’s disease)
• Women or men on chronic glucocorticoid therapy (equivalent to 5 mg or more of prednisone daily for three (3) months or longer).
• Postmenopausal women or men with osteoporosis by BMD criteria, if documentation of one or more vertebral fractures will alter clinical management.
Preparing For Your Bone Densitometry Exam
On your exam day, eat normally but please don’t take calcium supplements for at least 24 hours before your exam. Wear loose, comfortable clothing and avoid clothes with metal zippers, belts or buttons. Radiology & Imaging may ask you to remove some or all of your clothes and to wear a gown or robe during the exam. You may also have to remove jewelry, eyeglasses and any metal objects or clothing. Items like these can interfere with the x-ray images.
Let your physician know if you recently had a barium examination or have been injected with a contrast material for a computed tomography (CT) scan or radioisotope (nuclear medicine) scan.
Always inform your physician or the Radiology & Imaging technologist if there is any possibility that you are pregnant.
What a Bone Densitometry Exam Is
Like
You lie on a padded table. For a Central DXA exam, which measures bone density in the hip and spine, the x-ray generator is below you and an imaging device, or detector, is above. To assess your spine, your legs are supported on a padded box to flatten your pelvis and lower (lumbar) spine. To assess the hip, a technologist will place your foot in a brace that rotates your hip inward. In both cases, the detector slowly passes over, generating images on a computer monitor. Most exams only take 10-20 minutes and it’s important to remain still throughout the exam.
Benefits & Risks
Bone densitometry is simple, quick and noninvasive. It doesn’t require any anesthesia. The amount of radiation used is very small—significantly less than the dose of a standard chest x-ray.
With any x-ray procedure, there’s a slight chance of cancer from excessive exposure to radiation. However, the benefit of an accurate diagnosis far outweighs the risk. Women should always inform their physician or the Radiology & Imaging technologist if there is any possibility that they are pregnant.
Limits of Bone Densitometry
Bone densitometry cannot predict with 100% certainty if you will experience a fracture in the future. However, it can provide strong indications of your risk of a future fracture.
Despite its effectiveness in measuring bone strength, bone densitometry or DXA is of limited use for people with a spinal deformity or for people who have had spinal surgery. If you have vertebral compression fractures or osteoarthritis, your condition may interfere with the test’s accuracy. In these instances, another test may be performed, such as a forearm bone densitometry.
We Subspecialize In Reading Bone Images
Radiology & Imaging uses state-of-the-art equipment that provides exceptional diagnostic detail. Our body imaging radiologists or musculoskeletal radiologists specialize in reading bone densitometries which means more expertise and experience is at work for you.
Post time: Mar-07-2023